Saturday, 26 October 2019
Sunday, 16 June 2019
Vestibular Schwannomas
Definition
Arises from Schwann cells
May arise anywhere along the course of the axons of the eighth cranial nerve from the glial-Schwann sheath junction (Obersteiner-Redlich zone i.e. a root entry zone) up until their terminations within the auditory and vestibular end organs.
Most commonly within the most lateral portions of the CP angle or the internal auditory canal
Most commonly arises from inferior vestibular nerve. (and thus dispace VII anteriorly in 75%) <5% from cochlear nerve.
Aetiology
Ionising radiation
NF2 (FMH or de novo in c. 50%).
NF2 mosaicism also seen (mixture of cells).
Epidemiology
Rule of 8s
8th cranial nerve
8% of intracranial tumours
80% of CP angle tumours
Remaining 20% mostly meningiomas(10%), epidormoid (5%) Rarely facial nerve neuroma, metastatic lesion, vascular lesion (aneurysm/AVM) or lipoma, arachnoid cyst etc.
Pathology
In 60% of sporadic cases there is an inactivating mutation of the NF2 tumour suppressor gene (MERLIN)- germline in NFS, somatic in VS.
Benign
Antoni types A and B fibres
H&E stain
A cellular Antoni A area is seen on the right of the image. A paucicellular Antoni B area is seen on the left
Clinical Features
Investigations
MRI + gad + FIESTA (for anatomy)
Fine cut CT for surgical planing (e.g. pneumatization, IAC anatomy and jugular bulb location- may be high riding). High riding i.e. higher than inferior IAC.
PTA + speech discrimination
Left ear sensorineural hearing loss due to vestibular schwannoma. With sensorineural hearing loss, there is no significant difference in threshold between air and bone conduction.
The 50/50 rule is frequently quoted i.e. individuals with a PTA average greater than 50 dB and speech discrimination less than 50% do not have useful or salvageable hearing.
There is a Gardner-Robertson scale
Hearing preservation strongly correlated with tumour size.
Widened IAM is seen
Surgical Anatomy
Sigmoid and inferior petrosal sinuses empty into the jugular bulb, which continues as IJV. Occpuies posteriolateral aspect of the jugular foramen.
Arises from Schwann cells
May arise anywhere along the course of the axons of the eighth cranial nerve from the glial-Schwann sheath junction (Obersteiner-Redlich zone i.e. a root entry zone) up until their terminations within the auditory and vestibular end organs.
Most commonly within the most lateral portions of the CP angle or the internal auditory canal
Most commonly arises from inferior vestibular nerve. (and thus dispace VII anteriorly in 75%) <5% from cochlear nerve.
Aetiology
Ionising radiation
NF2 (FMH or de novo in c. 50%).
NF2 mosaicism also seen (mixture of cells).
Epidemiology
Rule of 8s
8th cranial nerve
8% of intracranial tumours
80% of CP angle tumours
Remaining 20% mostly meningiomas(10%), epidormoid (5%) Rarely facial nerve neuroma, metastatic lesion, vascular lesion (aneurysm/AVM) or lipoma, arachnoid cyst etc.
Pathology
In 60% of sporadic cases there is an inactivating mutation of the NF2 tumour suppressor gene (MERLIN)- germline in NFS, somatic in VS.
Benign
Antoni types A and B fibres
H&E stain
A cellular Antoni A area is seen on the right of the image. A paucicellular Antoni B area is seen on the left
Verocay bodies (soldiers in a line) also classic.
S-100 antibody on immunohistochemical staining (vs. EMA for meningiomas).
Most grow slowly e.g. 2mm/year but some do not grow and others fast.
Clinical Features
Most present with unilateral sensorineural hearing loss.
Typically speech discrimination will be reduced out of proportion to the PTA.
Disequilibrium is seen, but true vertigo is rare.
High pitched tinnitus
Typically gradual hearing loss
CNV and VII symptoms once tumour >2cm
Brainstem symptoms with larger tumours (>4cm)
MRI + gad + FIESTA (for anatomy)
Fine cut CT for surgical planing (e.g. pneumatization, IAC anatomy and jugular bulb location- may be high riding). High riding i.e. higher than inferior IAC.
PTA + speech discrimination
Left ear sensorineural hearing loss due to vestibular schwannoma. With sensorineural hearing loss, there is no significant difference in threshold between air and bone conduction.
The 50/50 rule is frequently quoted i.e. individuals with a PTA average greater than 50 dB and speech discrimination less than 50% do not have useful or salvageable hearing.
There is a Gardner-Robertson scale
Hearing preservation strongly correlated with tumour size.
Widened IAM is seen
Surgical Anatomy
Sigmoid and inferior petrosal sinuses empty into the jugular bulb, which continues as IJV. Occpuies posteriolateral aspect of the jugular foramen.
Grade 1 tumors involve only the internal
auditory canal.
Grade 3 tumor fills the entire cerebellopontine angle.
Grade 4 tumor displaces the brainstem and
adjacent cranial
nerves.
NB IAM also contains labyrinthine artery, branch of AICA (from basilar)
Management
Observation
Irradiation (Principally SRS)
Surgery (Retrosigmoid vs Trans-lab. vs middle-fossa).
1) Watch and wait (20% of pts)
a) Normal growth 1-10 mm/year
b) Only 17% if intracannalicular tumours grow outside meatus
c) 6% decrease in size
d) Complications of treatment go up if >15 mm in size
e) Annual audiometry: 50% will deteriorate to lower class over 4.6 years
2) SRS (13 gray)
a) Better for hearing preservation 81%, 77% and 66% at 3, 5 and 10 yrs
b) Facial nerve preservation 98%
c) Delayed improvement in vertigo
d) Max size c.3cm
SRS likely prevents further tumor growth by causing obliterative endarteritis of the vessels supplying the tumour. Probably the best strategy for most tumours under 3cm.
3) EBRT
4) Surgery
Middle fossa typically for small, lateral intracanalicular tumours that do not extent significantly into CP angle. Good for hearing preservation, but risk of seizures from temporal lobe retraction.
Retrosigmoid may preserve hearing but unlikely if >1cm (33%) and v unlikely if greater than 2cm (6%).
Translab sacrifices hearing, has a higher rate of CSF leak and takes longer. Exposure is also limited (possible maximum size).
However, possibly lower rate of VII injury, less risk to cerebellum (retraction not needed) and lower cranial nerves. Patients are not as generally unwell from blood in CSF.
Overall recurrence rate 5-10% post surgery. Generally f/u for 10 years.
Monday, 15 April 2019
Chiari Malformations
Clinical Features
Congenital or Acquired (e.g. LP shunts, CSDH, hydrocephalus).
Chiari 1- tonsillar descent >5mm (3-5mm borderline) below foramen magnum (or McRae basion-opisthion). A/w Syrinx in >30%. (also scoliosis, hydrocephalus in <10%, small p fossa, thickened occipital bone, low lying tent, basilar invagination)
Chiari 2- tonsillar, vermian, medulla/brainstem and 4th ventricular descent. A/w cervicomedullary kinking, myelomeningocele and hydrocephalus in most cases. Numerous other associations e.g. tectal beaking etc.
Chiari 3- occpital encephalocele
Chiari 4- cerebella hypoplasia)
Chiari 0- syrinx without Chiari
1/3 asymptomatic 2/3 have pain- classically suboccipital strain headaches. May c/o limb weakness/wasting.
o/e 3 patterns:
- FM compression signs i.e. ataxia, corticospinal (usually unilateral) and sensory deficits, cerebellar signs, lower cranial nerve palsies.
- Central cord syndrome (dissociated sensory loss, occasional weakness, long tract signs.
- Cerebellar syndrome (truncal and limb ataxia, nystagmus, dysarthria).
Nystamus is classically downbeat. May have Lhermitte's sign.
Important to note presence/absence of brainstem signs e.g. dysphagia o/e, palatal movements (uvula position) and tongue wasting.
Reflexes may be brisk in Chiari but should be reduced with syrinx (LMN phenomenon). As syrinx is usually cervical 'cape like' dissociated sensory loss (loss of spinothalamic pain/temp but preserved LT/JPS/vibration) typically seen. Also loss of temperature hence injuries/ulcers (ask can they tell hot from cold water). Look for atrophy e.g. of hand and arm.
Investigations
MRI whole spine
Cine or CSF flow may be requested
Empty sella may be seen on MR
Indications for surgery
Symptoms
Syrinx
Surgical Mangement (FMD)
Small suboccipital craniectomy e.g. 1cm (max 2cm) to avoid cerebellar slumping.
In paediatrics, bony decomression alone sometimes attempted (USS can be used to assess flow).
Open dura in Y shape
Other measures controversial e.g. opening arachnoid, lysing bands, identifying obex/Magendie, diathermy/subpial dissection to tonsills and tonsillopexy) +/- duroplasty.
Bleeding from marginal sinus may be irritating. Can be packed e.g. with muslin.
Complications include: cerebellar ptosis, CSF leak, brainstem injury/stroke (e.g. PICA), apnoea/respiratory depression.
Congenital or Acquired (e.g. LP shunts, CSDH, hydrocephalus).
Chiari 1- tonsillar descent >5mm (3-5mm borderline) below foramen magnum (or McRae basion-opisthion). A/w Syrinx in >30%. (also scoliosis, hydrocephalus in <10%, small p fossa, thickened occipital bone, low lying tent, basilar invagination)
Chiari 2- tonsillar, vermian, medulla/brainstem and 4th ventricular descent. A/w cervicomedullary kinking, myelomeningocele and hydrocephalus in most cases. Numerous other associations e.g. tectal beaking etc.
Chiari 3- occpital encephalocele
Chiari 4- cerebella hypoplasia)
Chiari 0- syrinx without Chiari
1/3 asymptomatic 2/3 have pain- classically suboccipital strain headaches. May c/o limb weakness/wasting.
o/e 3 patterns:
- FM compression signs i.e. ataxia, corticospinal (usually unilateral) and sensory deficits, cerebellar signs, lower cranial nerve palsies.
- Central cord syndrome (dissociated sensory loss, occasional weakness, long tract signs.
- Cerebellar syndrome (truncal and limb ataxia, nystagmus, dysarthria).
Nystamus is classically downbeat. May have Lhermitte's sign.
Important to note presence/absence of brainstem signs e.g. dysphagia o/e, palatal movements (uvula position) and tongue wasting.
Reflexes may be brisk in Chiari but should be reduced with syrinx (LMN phenomenon). As syrinx is usually cervical 'cape like' dissociated sensory loss (loss of spinothalamic pain/temp but preserved LT/JPS/vibration) typically seen. Also loss of temperature hence injuries/ulcers (ask can they tell hot from cold water). Look for atrophy e.g. of hand and arm.
Investigations
MRI whole spine
Cine or CSF flow may be requested
Empty sella may be seen on MR
Indications for surgery
Symptoms
Syrinx
Surgical Mangement (FMD)
Small suboccipital craniectomy e.g. 1cm (max 2cm) to avoid cerebellar slumping.
In paediatrics, bony decomression alone sometimes attempted (USS can be used to assess flow).
Open dura in Y shape
Other measures controversial e.g. opening arachnoid, lysing bands, identifying obex/Magendie, diathermy/subpial dissection to tonsills and tonsillopexy) +/- duroplasty.
Bleeding from marginal sinus may be irritating. Can be packed e.g. with muslin.
Complications include: cerebellar ptosis, CSF leak, brainstem injury/stroke (e.g. PICA), apnoea/respiratory depression.
Thursday, 14 March 2019
Thalamic Nuclei
Thalamic Nuclei

If you get orientated, they are largely as they say on the tin
Pulvinar is posterior (means cushion- you sit on it with your posterior)
The ventral 'belly' side faces outwards *laterally).


If you get orientated, they are largely as they say on the tin
Pulvinar is posterior (means cushion- you sit on it with your posterior)
The ventral 'belly' side faces outwards *laterally).


Wednesday, 13 March 2019
Parasympathetics
Parasympathetics





| Feature | Sympathetic NS | Parasympathetic NS |
| Summary of responses | Fight or flight | Rest and digest |
| Spinal cord distribution | Thoracolumbar | Craniosacral |
| Preganglionic neurone | Short | Long |
| Preganglionic neurotransmitter | Acetylcholine (Ach, cholinergic) | Acetylcholine (Ach, cholinergic) |
| Postganglionic neurone | Long | Short |
| Postganglionic neurotransmitter | Noradrenaline (NA, adrenergic) in most cases* | Acetylcholine (Ach, cholinergic) |
*Sweat being an exception
Efferent i.e. motor
Afferent i.e. towards the CNS so sensory
Parasympathetic motor efferents—This system is divided into cranial and sacral components, and parasympathetic efferents only synapse with postganglionic cells close to or within target viscera (allowing local discrete responses)
4 main parasympathetic nuclei (III, VII, IX, X) with synapses in 4 ganglia (NB ganglia are outside CNS)
NB Most ganglia are associated with some sensory and sympathetic nerves – these do not synapse in the ganglia, they merely travel through it.
1. Cilliary (parasympathetic eye)
Supplied by fibres from Edinger-Westphal nucleus (a/w CNIII)
Function: pupil constriction and accommodation
2. Pterygopalatine Ganglion (aka sphenopalatine) in pterygopalatine fossa (cries/lubricates nasopharynx)
Supplied by superior salivatory nuclues (a/w CN VII) via GSPN and Vidian nerve.
Function: secretomotor innervation to lacrimal gland, mucous glands of nasal cavity, nasopharynx and palate.

3. Submandibular ganglion (salivates)
Suspended from lingual nerve
Supplied by superior salivatory nucleus (a/w CN VII)
Function: Secretomotor innervation to the submandibular and sublingual salivary glands
4. OTic Ganglion (parOTid - salivates)
Inferior to foramen ovale
Supplied by inferior salivatory nuclues (a/w CN IX)
Innervates parotid

NB Vagus (X) does not innervate head and neck structures - only thorax and abdomen.
| Nucleus | Pre-ganglionic | Ganglion | Post-ganglionic | Target organs |
| Edinger-Westphal (Oculomotor nerve) | Travels with the motor root of the oculomotor nerve | Ciliary ganglion | Travels via the short ciliary nerves | Sphincter pupilliae
Ciliary muscles
|
| Superior salivatory nucleus (Facial nerve) NB VII above IX hence sup and inf (both salivate) | Travels with the greater petrosal nerve and the nerve of the pterygoid canal | Pterygopalatine ganglion | Hitchhikes on branches of the maxillary nerve | Lacrimal gland
Nasopharynx
Palate
Nasal cavity
|
| Travels within the chorda tympani, a branch of the facial nerve | Submandibular ganglion | Fibres travel directly to target organs | Sublingual and submandibular glands | |
| Inferior salivatory nucleus (Glossopharyngeal nerve) | Travels within the lesser petrosal nerve | Otic ganglion | Hitchhikes on the auriculotemporal nerve | Parotid gland |
| Dorsal vagal motor nucleus (vagus nerve) | Travels within the vagus nerve | Many – located within the target organs | n/a | Smooth muscle of the trachea, bronchi and gastro-intestinal tract |
Tuesday, 12 March 2019
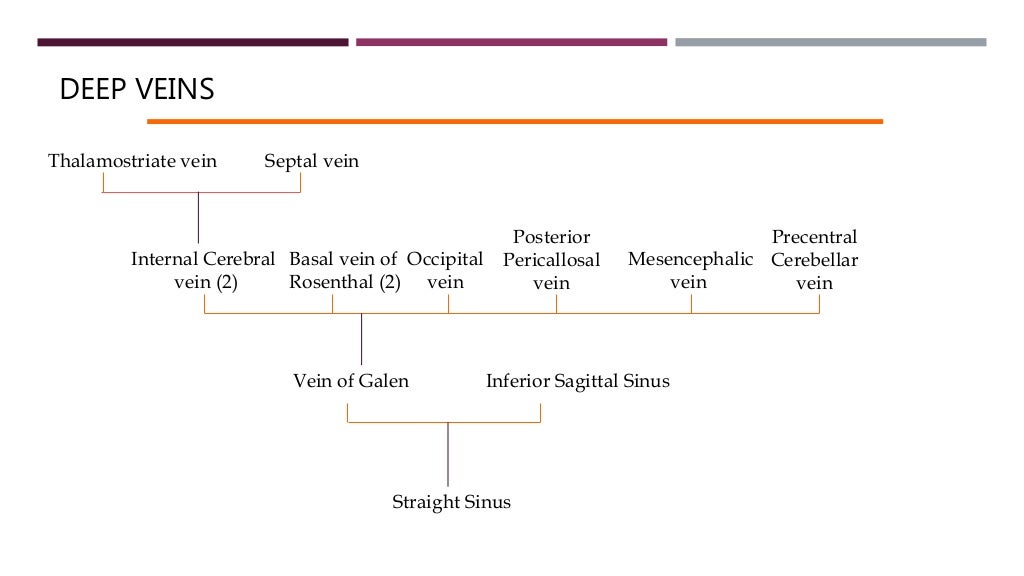
Cerebral Venous System
Cerebral Sinuses and Veins
There are 11 venous sinuses in total, between periostial and meningeal layers of dura.
Veins of significance include Thalamostriate, Superior Anastomotic Vein (of Trolard), Internal Cerebral Vein, Great Cerebral Vein (of Galen), Basal Vein (of Rosenthal), Inferior Anastomotic Vein (of Labbe), transverse vein, Middle Cerebral Veins (of Sylvius)- Deep and Superficial, Anterior cerebral vein,
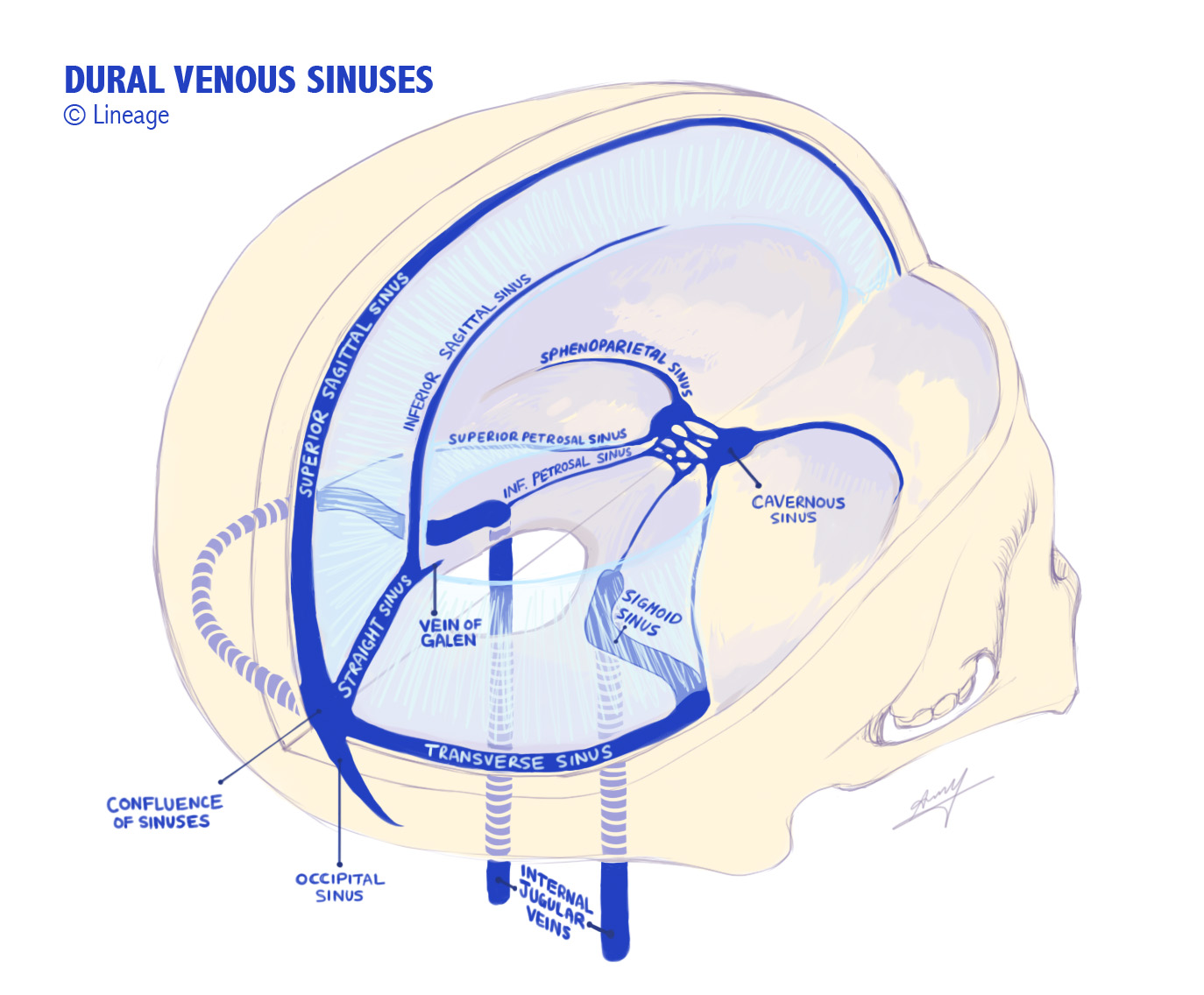
Right transverse sinus is usually dominant and typically receives superficial blood- via continuation of SSS; left TS typically drains deep brain
NB inferior petrosal sinus sampling (to measure ATCH levels) is a clue that this drains pituitary.
Veins are located in subarachnoid space and divided into superficial and deep systems.
Superficial Veins
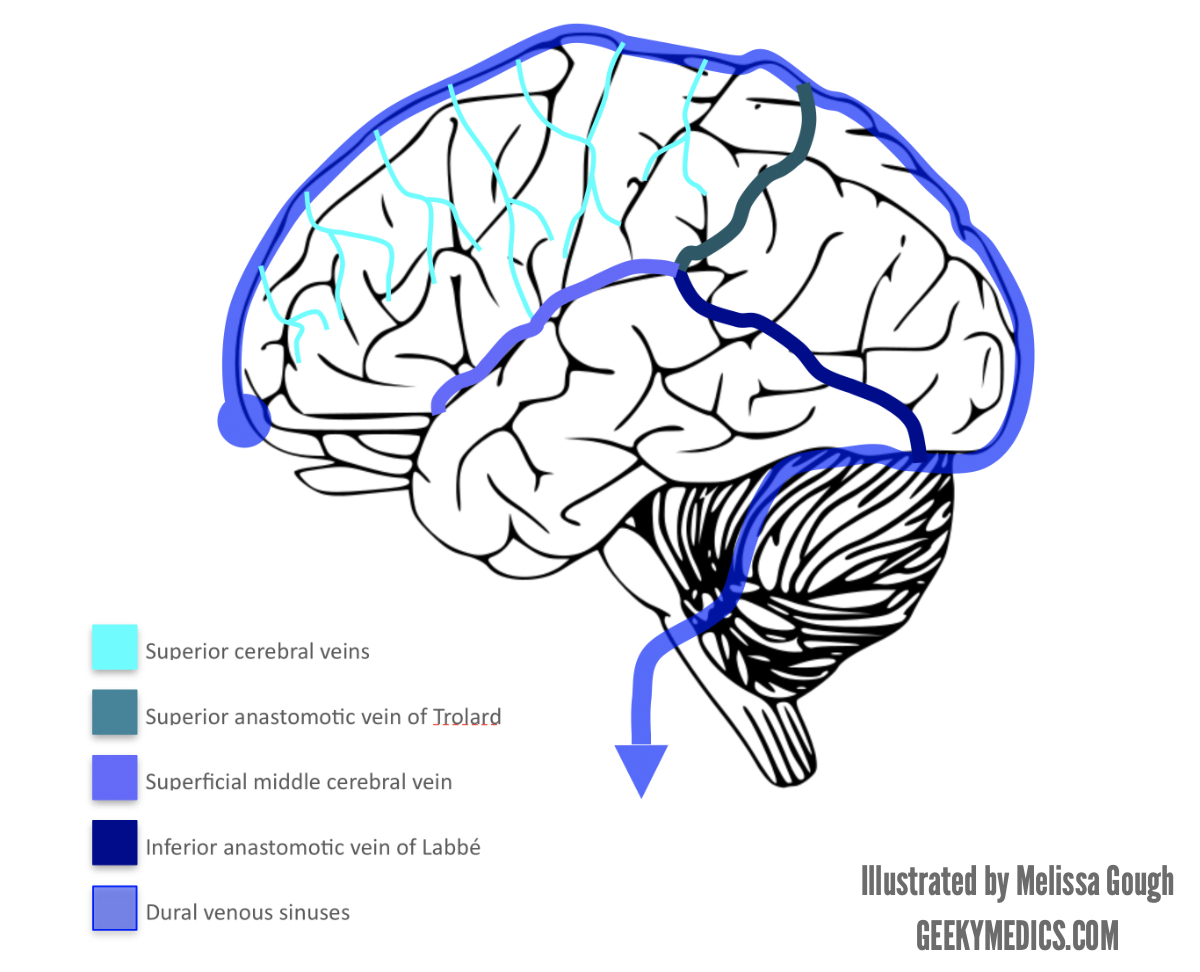
Trolard, Labbe and Sylvius (superficial) all meet up.
Visual Pathways
Visual Pathways
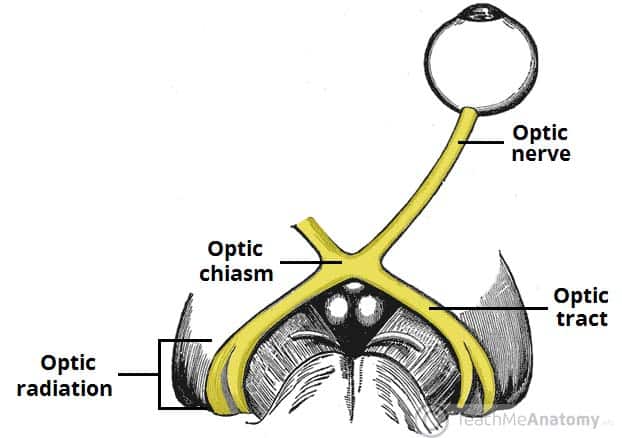

Blue arrows indicate Meyer's Loop.

Optic nerve is developed from the optic vesicle.
Originates from retinal ganglion cell axons, enters the cranial cavity via optical canal, passing through tendinous ring annulus of Zinn.

"2, 3 n 6" pass within the annulus, n being nasociliary nerve (i.e. V1 branch).

Meyer's loop is anterior, inferior and temporal; central bundle abuts lateral ventricle; the dorsal bundle is superior and parietal (Baum's loop). Meyer's loop produces pie in the sky deficit.
NB Nasal fibres cross at the chiasm, temporal don't (you cross your eyes at your nose).


This demonstrates the geniculate pathway conscious visual processing (incorporating the LGN of the thalamus)
There are also extrageniculate pathways, which project to: pretectal nucleus (midbrain- pupillary reflexes), superior colliculus (midbrain- coordinated reflexive head and eye movements), suprachiasmatic nucleus (hypothalamus- circadian cycles).

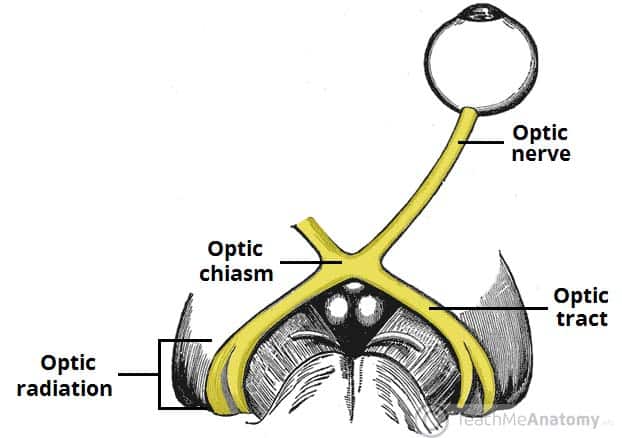
Blue arrows indicate Meyer's Loop.

Optic nerve is developed from the optic vesicle.
Originates from retinal ganglion cell axons, enters the cranial cavity via optical canal, passing through tendinous ring annulus of Zinn.

"2, 3 n 6" pass within the annulus, n being nasociliary nerve (i.e. V1 branch).
Meyer's loop is anterior, inferior and temporal; central bundle abuts lateral ventricle; the dorsal bundle is superior and parietal (Baum's loop). Meyer's loop produces pie in the sky deficit.
NB Nasal fibres cross at the chiasm, temporal don't (you cross your eyes at your nose).


This demonstrates the geniculate pathway conscious visual processing (incorporating the LGN of the thalamus)
There are also extrageniculate pathways, which project to: pretectal nucleus (midbrain- pupillary reflexes), superior colliculus (midbrain- coordinated reflexive head and eye movements), suprachiasmatic nucleus (hypothalamus- circadian cycles).

Sunday, 24 February 2019
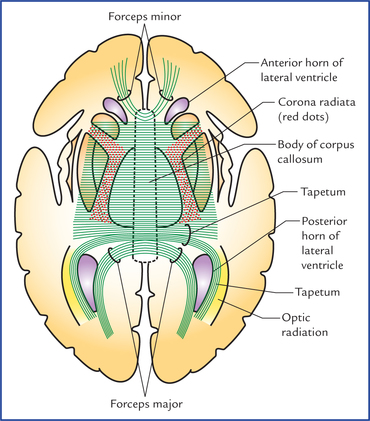
Cranial Projection and Association Tracts and Limbic System
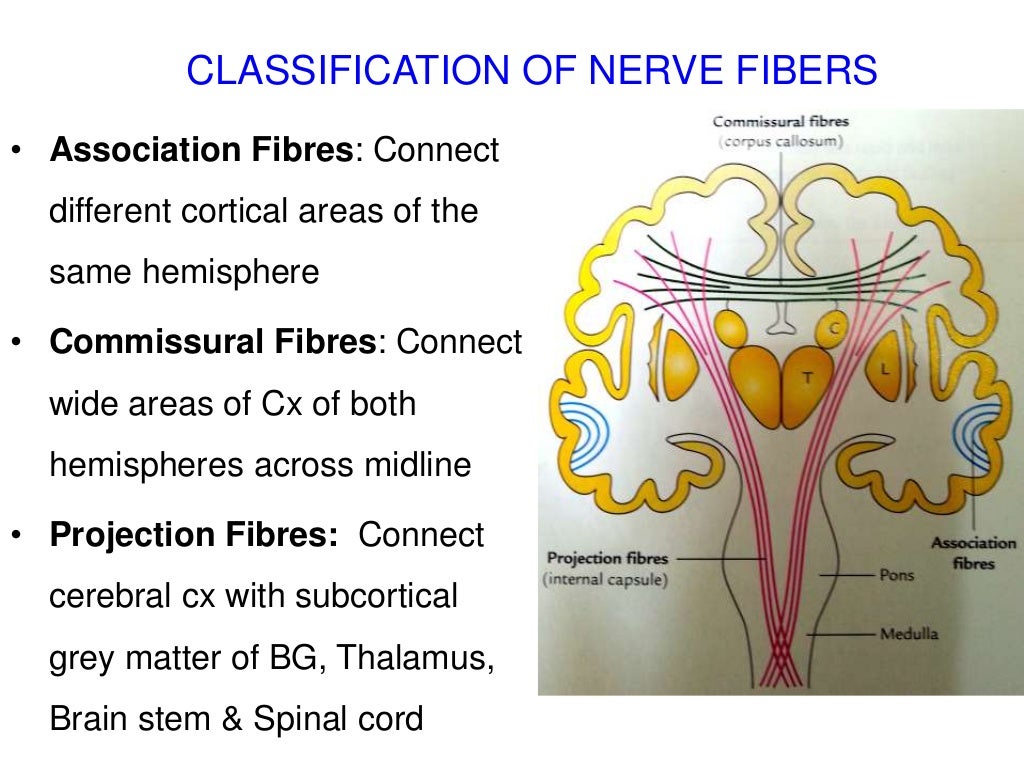

Bundles implies long association fibres

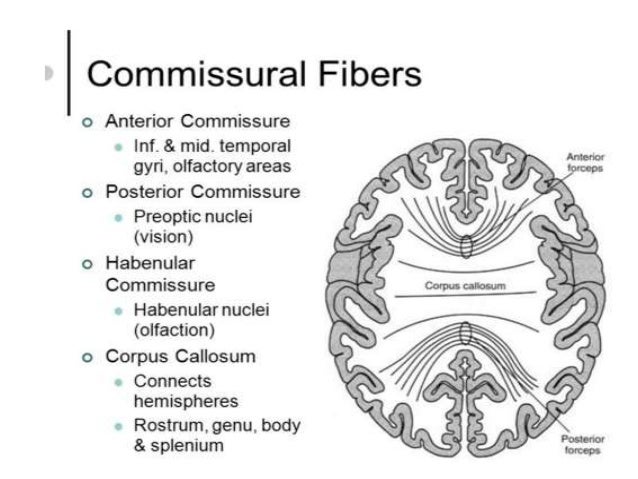

Corpus callosum fibres


VA- ventral anterior
VL - ventral lateral

NB Lentiform nucleus = GP + putamen
Tegmentum (Lat- Covering). Forms floor of midbrain cf.
Tectum (Lat- Roof). Forms roof of midbrain.
Stria (Lat- Stripe)
Fasciculus (Lat- Bundle)
Tapetum (Lat- Tapestry/rug)
Habenula (Lat- reins). Denotes stalk of pineal gland and neighbouring neurons.


Resembles a tapestry; the carpet of the brain. Primarily formed by decussating fibres of the splenium.
Septal nuclei are by septum pellucidum. Role in pleaseure/reward like Nucleus Accumbus.
Limbic System- a ring of memory and emotion (like a wedding ring).
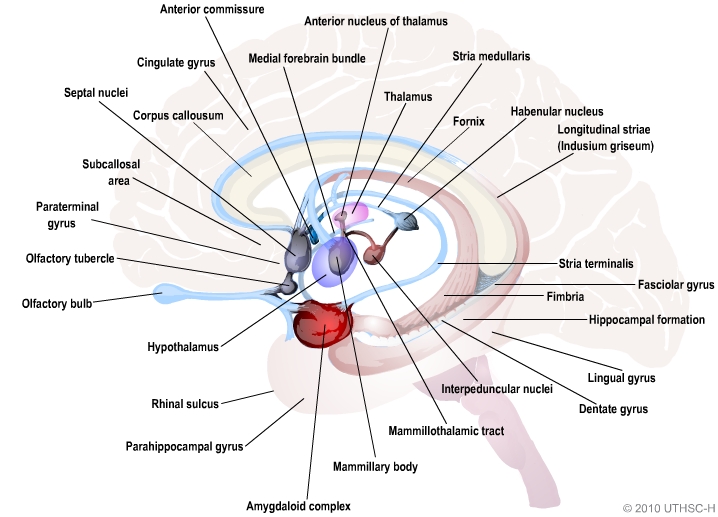
Simplified:
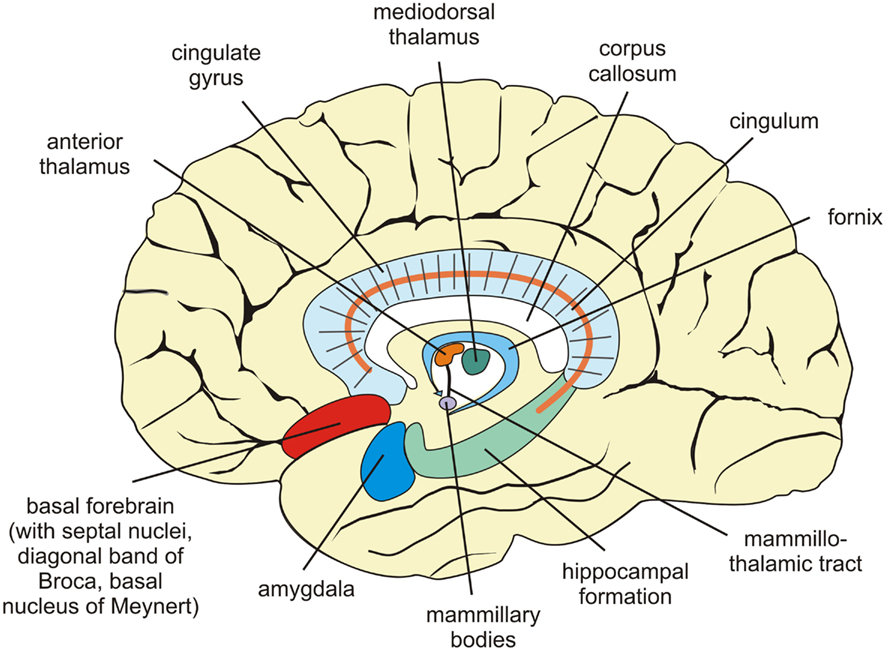
Deontes a conerstone of memory processing/consolidation

Indusium (tunic/shirt) griseum is membranous layer of grey matter which covers the corpus callosum.
Subscribe to:
Comments (Atom)



















