Definition
Arises from Schwann cells
May arise anywhere along the course of the axons of the eighth cranial nerve from the glial-Schwann sheath junction (Obersteiner-Redlich zone i.e. a root entry zone) up until their terminations within the auditory and vestibular end organs.
Most commonly within the most lateral portions of the CP angle or the internal auditory canal
Most commonly arises from inferior vestibular nerve. (and thus dispace VII anteriorly in 75%) <5% from cochlear nerve.
Aetiology
Ionising radiation
NF2 (FMH or de novo in c. 50%).
NF2 mosaicism also seen (mixture of cells).
Epidemiology
Rule of 8s
8th cranial nerve
8% of intracranial tumours
80% of CP angle tumours
Remaining 20% mostly meningiomas(10%), epidormoid (5%) Rarely facial nerve neuroma, metastatic lesion, vascular lesion (aneurysm/AVM) or lipoma, arachnoid cyst etc.
Pathology
In 60% of sporadic cases there is an inactivating mutation of the NF2 tumour suppressor gene (MERLIN)- germline in NFS, somatic in VS.
Benign
Antoni types A and B fibres
H&E stain
A cellular
Antoni A area is seen on the right of the image. A paucicellular
Antoni B area is seen on the left
Verocay bodies (soldiers in a line) also classic.
S-100 antibody on immunohistochemical staining (vs. EMA for meningiomas).
Most grow slowly e.g. 2mm/year but some do not grow and others fast.
Clinical Features
Most present with unilateral sensorineural hearing loss.
Typically speech discrimination will be reduced out of proportion to the PTA.
Disequilibrium is seen, but true vertigo is rare.
High pitched tinnitus
Typically gradual hearing loss
CNV and VII symptoms once tumour >2cm
Brainstem symptoms with larger tumours (>4cm)
Investigations
MRI + gad + FIESTA (for anatomy)
Fine cut CT for surgical planing (e.g. pneumatization, IAC anatomy and jugular bulb location- may be high riding). High riding i.e. higher than inferior IAC.
PTA + speech discrimination
Left ear sensorineural hearing loss due to vestibular schwannoma. With sensorineural hearing loss, there is no significant difference in threshold between air and bone conduction.
The 50/50 rule is frequently quoted i.e. individuals with a PTA average greater than 50 dB and speech discrimination less than 50% do not have useful or salvageable hearing.
There is a Gardner-Robertson scale
Hearing preservation strongly correlated with tumour size.
Widened IAM is seen
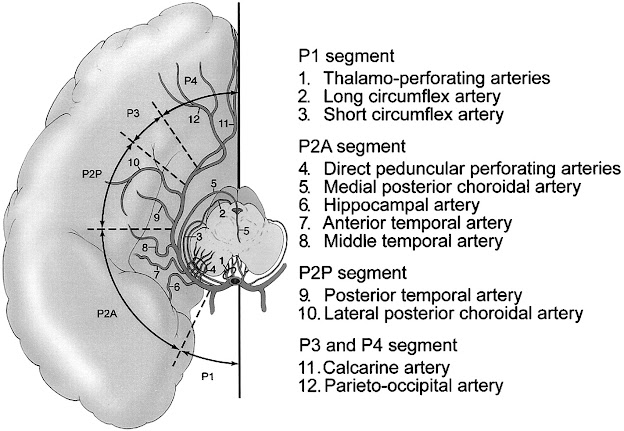
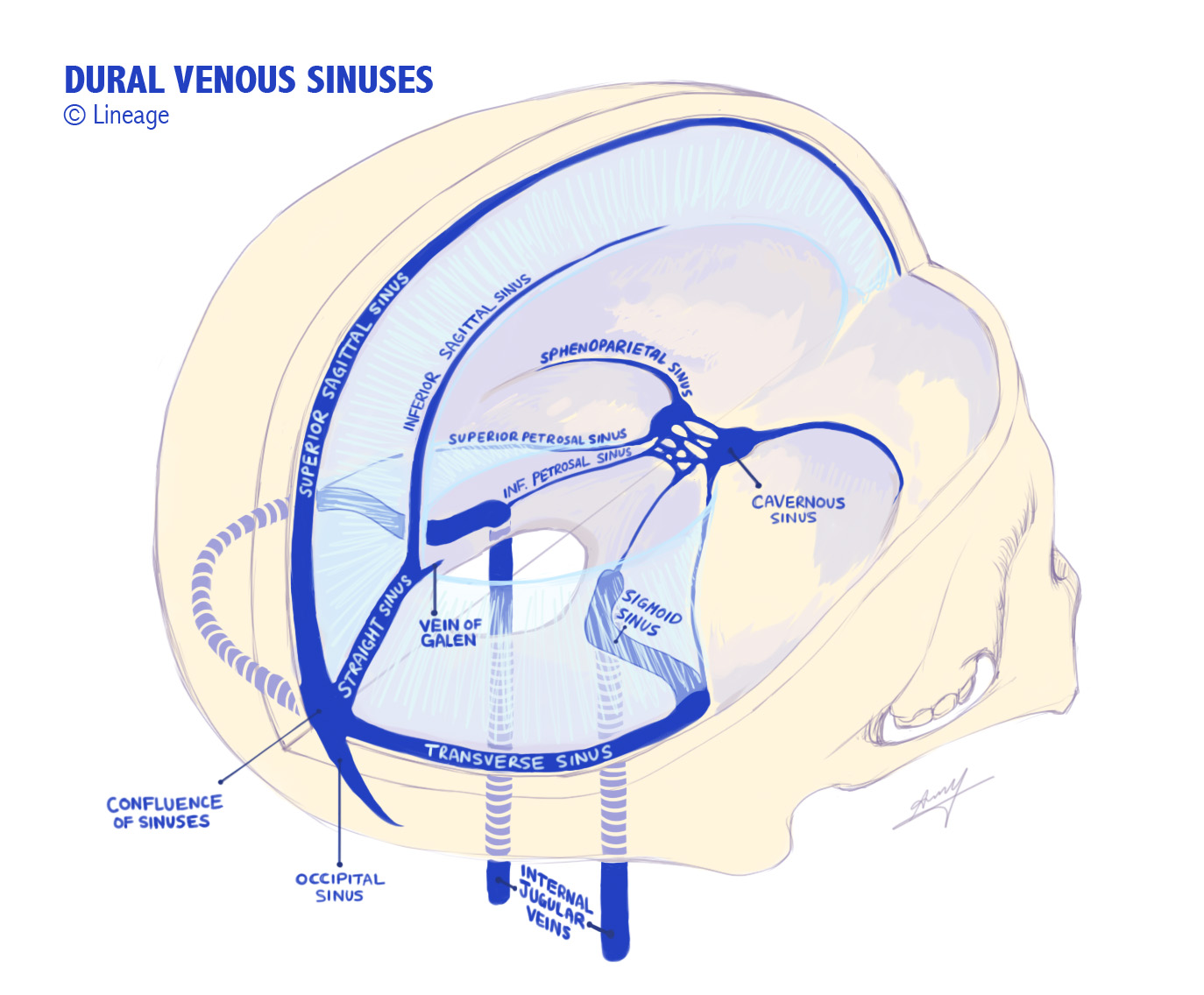
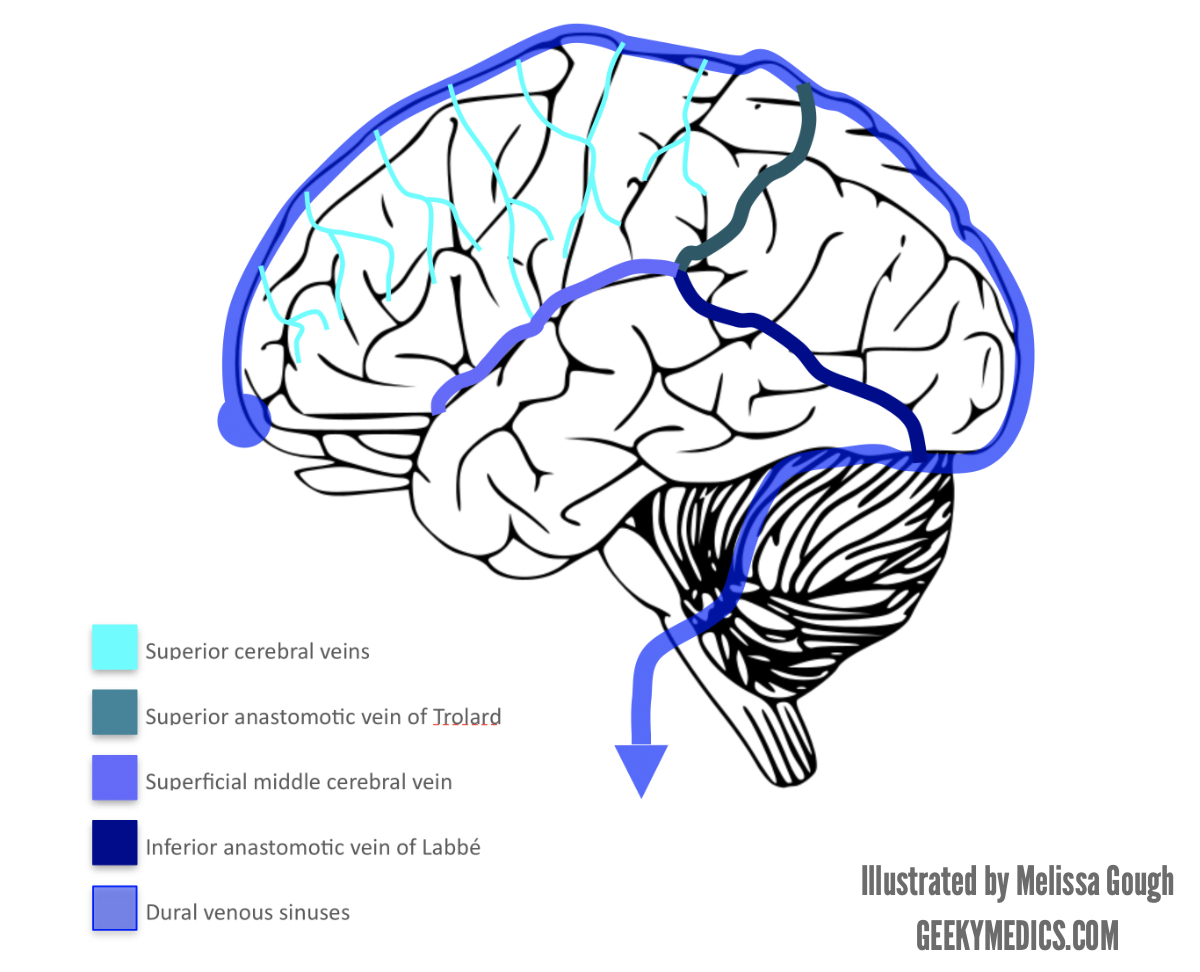
Surgical Anatomy
Sigmoid and inferior petrosal sinuses empty into the jugular bulb, which continues as IJV. Occpuies posteriolateral aspect of the jugular foramen.
 Koos grading
Koos grading
Grade 3 tumor fills the entire cerebellopontine angle.
NB IAM also contains labyrinthine artery, branch of AICA (from basilar)
Management
Observation
Irradiation (Principally SRS)
Surgery (Retrosigmoid vs Trans-lab. vs middle-fossa).
1) Watch and wait (20% of pts)
a) Normal growth 1-10 mm/year
b) Only 17% if intracannalicular tumours grow outside meatus
c) 6% decrease in size
d) Complications of treatment go up if >15 mm in size
e) Annual audiometry: 50% will deteriorate to lower class over 4.6 years
2) SRS (13 gray)
a) Better for hearing preservation 81%, 77% and 66% at 3, 5 and 10 yrs
b) Facial nerve preservation 98%
c) Delayed improvement in vertigo
d) Max size c.3cm
SRS likely prevents further tumor growth by causing obliterative endarteritis of the vessels supplying the tumour. Probably the best strategy for most tumours under 3cm.
3) EBRT
4) Surgery
Middle fossa typically for small, lateral intracanalicular tumours that do not extent significantly into CP angle. Good for hearing preservation, but risk of seizures from temporal lobe retraction.
Retrosigmoid may preserve hearing but unlikely if >1cm (33%) and v unlikely if greater than 2cm (6%).
Translab sacrifices hearing, has a higher rate of CSF leak and takes longer. Exposure is also limited (possible maximum size).
However, possibly lower rate of VII injury, less risk to cerebellum (retraction not needed) and lower cranial nerves. Patients are not as generally unwell from blood in CSF.
Overall recurrence rate 5-10% post surgery. Generally f/u for 10 years.